What Are the Surgery Options to Treat My Trigger Finger?
Trigger finger is a common problem that can cause a locking sensation and pain in one or more fingers. This condition tends to be more frequent in the thumb, middle, and ring finger. This disorder is usually linked to repeatedly grasping or gripping a certain object (steering wheel while driving, a racket while playing tennis or badminton, or even a cellphone, for instance). This repetitive gripping eventually breaks down and swells the fat pad at the base of the finger. It’s precisely this swelling that causes the locking sensation and pain that you feel whenever you try to move your finger.
There are many conservative and at home treatments to help relieve your pain caused by trigger finger or thumb. Some of these remedies include resting, ice and hot therapy, exercises, stretches, anti-inflammatory medications, and immobilizing the finger with a trigger finger splint. Some try a steroid injection (most common treatment method) to the affected finger to help reduce inflammation.
Unfortunately, if none of these methods treats or reduces your pain, surgery is pursued. An estimated 85% of instances of trigger finger can be treated without surgery, though the odds of this go down if the condition goes untreated for six months or more. If left untreated, the finger has a chance of becoming permanently stuck in a bent position. But on the flip side, both types of surgery for trigger finger are relatively simple procedures that can usually be done on an outpatient basis.
There are two main types of trigger finger or thumb surgery: open and percutaneous. Both of these procedures involve the doctor “releasing,” or splitting the A1 pulley through which the tendon is having trouble passing. The difference between these trigger finger surgeries is how the doctor goes about doing so. Speak with your doctor about which surgery is the best option for you!
For those who have rheumatoid arthritis, neither of these surgeries may be performed. Instead, a tenosynovectomy is performed, which removes part of the tendon sheath.
Open Surgery for Trigger Finger or Thumb Pain
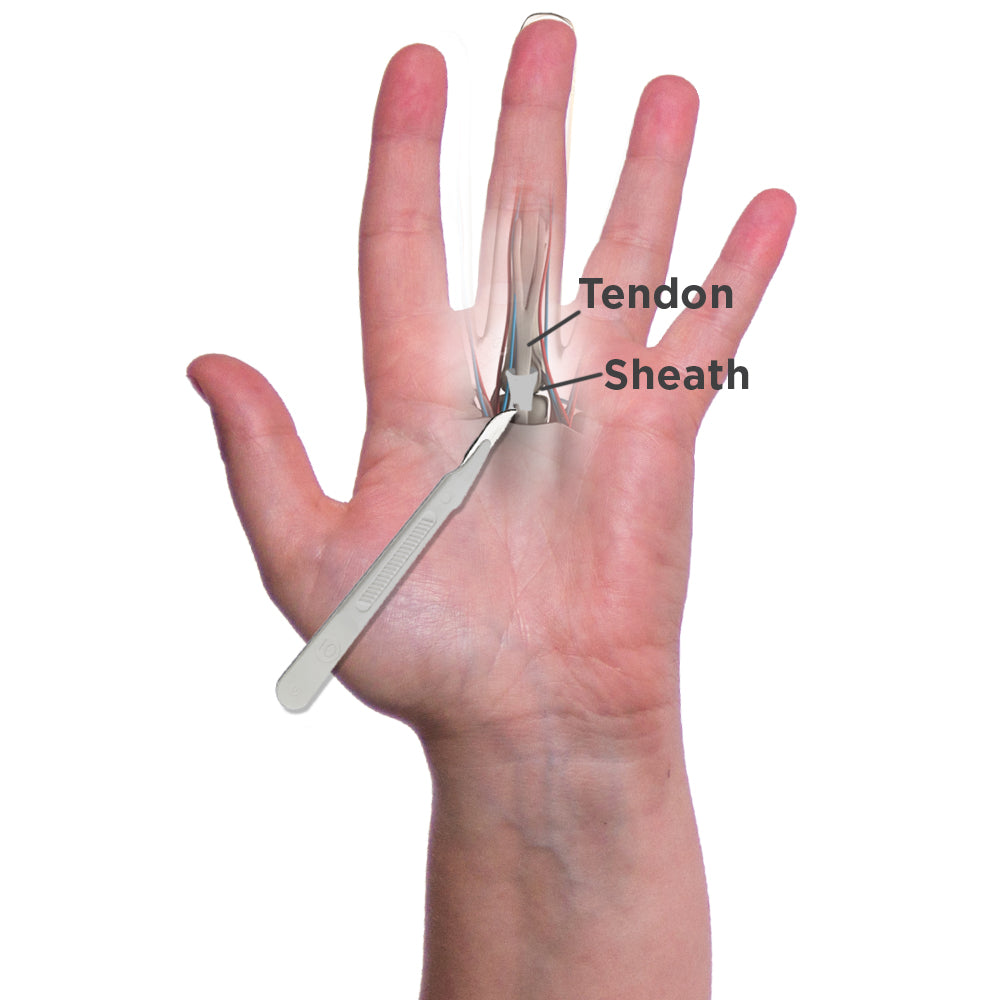
With open surgery, the doctor will usually use local or regional anesthesia to deaden the hand or arm (general anesthesia is sometimes used, though this raises the cost of trigger finger surgery). Then he or she will make a small incision to open up the hand to widen the tendon sheath. The surgeon will then close the wound with stitches and will cover the area with a bandage.
This is the preferred method for surgery to help treat trigger finger.
Percutaneous Surgery for Trigger Finger or Thumb Pain

For percutaneous trigger finger release surgery, instead of making an incision in your palm, the doctor will use a needle to break apart the blockage in the tendon sheath. Only a local anesthetic is usually needed and in some cases this procedure can be done in the doctor’s office, avoiding the extra trigger finger surgery cost of a hospital visit and surgery room, not to mention an anesthesia fee.
The downside of this less invasive percutaneous procedure is that the surgeon does not have a view of the pulley he or she is cutting; thus, this may raise the risk of trigger finger surgery complications such as digital nerve damage from a cut made in error. However, studies of percutaneous trigger finger release surgery have yielded as high as 100% success rates. The plus side of this surgery is that you will not have a scar or wound.
Can There Be Any Trigger Finger Surgery Complications?
Fortunately, trigger finger surgery is relatively a safe procedure. Depending on your specific case, there may be some complications that may arise after the infection including:
- Infection at the incision site
- Stiffness in the finger
- Scarring
- Nerve damage
How Long Is My Expected Recovery Time?
Trigger finger surgery recovery time varies based on each individual but is typically pretty quick. For open surgery, it usually takes four to six weeks to get back to unrestricted motion, while those who have had percutaneous trigger finger release will have a shorter recovery time, as there will be no wound in the palm to heal.
Whether you will need to take time off work to allow for trigger finger release surgery recovery time depends upon the nature of your job. If you do extensive manual labor, you may need to take three weeks off of work. On the other hand, if you have a light manual labor job such as a desk job, you may not need to take any time off to allow for recovery time for trigger finger surgery.
What Can I Do After Surgery For Trigger Finger?
Movement of the finger is possible and even recommended very soon after trigger finger surgery, though you must be careful as to what type of movement you do during recovery from trigger finger surgery. You should do trigger finger exercises after surgery with a focus on improving the range of motion of the finger rather than speed. Try avoiding forceful, repetitive motions of the finger.
You can engage in light daily activities, lifting, typing, writing, etc. in the first week following surgery so long as this is done in moderate doses. You should always pay attention to any pain or swelling after trigger finger surgery and stop doing any actions that increase these side effects. Keeping the hand above the waist as much as possible can also be helpful toward minimizing swelling after surgery. Using ice will help to lower swelling as well. Driving should not be a problem after trigger finger or thumb surgery and over the counter medications should be effective in reducing any pain.
In addition, wear a trigger finger splint during the night time to help protect your finger and during the day to help prevent forceful, repetitive movement of the finger.
Visit our orthopedic library to learn more about trigger finger and trigger thumb as well as alternative treatment options.