Isthmic & Degenerative Spondylolisthesis Surgery & Recovery Options

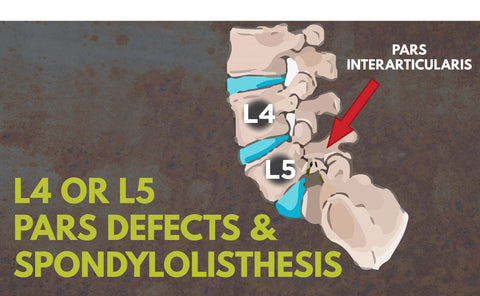
Spondylolisthesis is defined as one of your bones in your vertebra-sliding forward (referred to as anterolisthesis) or backward (referred to as retrolisthesis) over the bone next to it. This typically occurs at the fifth or fourth vertebra of the low back, with slippage of the fifth vertebra (L5) being the most common form of lumbar spondylolisthesis.
Surgery for spondylolisthesis is usually considered only after conservative modes of treatment, such as resting your back, wearing a spondylolisthesis brace and engaging in physical therapy, have failed to bring relief and the degree of slippage is advanced.
Back surgery for spondylolisthesis is usually only considered in instances of grade II (26-50% slippage), grade IV (76% to 100% slippage), or grade V (your vertebrae has completely unattached) spondylolisthesis. For grade II of spondylolisthesis, surgery is usually advised because it is a result of a trauma or fall to your spine that caused the slippage. Surgery will help to readjust your vertebrae.
Typically, for grade I and grade III, surgery is not common. Grade I spondylolisthesis is caused by a deformation of your spine that is present at birth. Over time, other regions in your spine adapt to this deformation, therefore having surgery may further harm your spine.
With wear-and-tear spondylolisthesis (grade III), a doctor will also consider the extent of arthritis (if applicable) before making a decision on degenerative spondylolisthesis surgery. With stress fracture caused by isthmic spondylolisthesis surgery, a doctor will consider how quickly the vertebra is slipping out of position. Isthmic spondylolisthesis, also known as spondylolysis, above the L5/S1 level surgery is more likely because the spine has more mobility in this lumbar region of the spine.
And even in such instances, you may not be a candidate for surgery, since such procedures involve a fair amount of risk. In addition to the degree of slippage, a doctor will also consider a patient’s age, health, and the severity of your symptoms in determining whether you are a candidate for back surgery for spondylolisthesis.

Regardless of whether you are in need of in cervical, thoracic or lumbar spondylolisthesis surgery, there are three main goals when it comes to surgery:
- To relieve pain stemming to an irritated nerve or spinal cord.
- To stabilize the spine in the problematic area.
- To improve the patient’s ability to function.
What Are Spondylolisthesis Surgery Options?
Surgery for spondylolisthesis typically involves a decompressive laminectomy procedure, possibly along with spinal fusion. A decompressive laminectomy surgery involves removing the roof of the vertebrae to create more space for the nerves. Sometimes all or part of an intervertebral disc must also be removed to ease pressure on the nerve root. Often, a laminectomy is done along with spinal fusion to improve the stability of the spine. This is often because a laminectomy can compromise the stability of the spine, plus spinal instability is often the cause of spondylolisthesis. Spinal fusion involves bone grafting and possibly the use of hardware such as rods, screws, etc. to internally fixate the spine, enabling it to heal. Surgery relieves the symptoms of spondylolisthesis at a success rate of roughly 85% to 90% of the patients.Risks of Surgery for Spondylolisthesis Treatment
But there are risks for spondylolisthesis surgery, which is why other, conservative spondylolisthesis therapy methods are the first line of treatment for this condition. Rare, but nevertheless possible, risks or complications of spondylolisthesis surgery include:- Infection
- Degenerative spondylolisthesis surgery bleeding
- Pain at graft site
- Recurrence of the symptoms
- Pseudarthrosis (not enough bone formation, in which case another surgery may be necessary; more common with smokers)
- Nerve or blood vessel damage
- Blood clots in the legs
Spondylolisthesis Physical Therapy and Recovery
While some patients require several days of hospitalization following a laminectomy, others are able to go home the same day. During spondylolisthesis surgery recovery, you will have to limit activities that involve bending, stooping or lifting for several weeks. You may also need some help getting out of bed or walking for a few days. Most often, you can return to light activity within a few days or weeks.
If you also had spinal fusion surgery, your spondylolisthesis recovery time will be longer as it will take between two and four months for the fused bone to solidify. However, you will typically feel better much sooner than that.
To help ensure a speedy and full recovery from one or both of these procedures, spondylolisthesis physical therapy exercises will likely be necessary. These are highly focused on stabilization exercises and hamstring stretching for lumbar spondylolisthesis. In line with this, physical therapy exercises for spondylolisthesis often work to strengthen and improve the flexibility of the abdomen and back muscles so that they can stabilize the spine and reduce pain.
 You can also wear a spondylolisthesis support brace to help immobilize your spine and prevent further injury.
You can also wear a spondylolisthesis support brace to help immobilize your spine and prevent further injury.