Patellofemoral Pain Syndrome
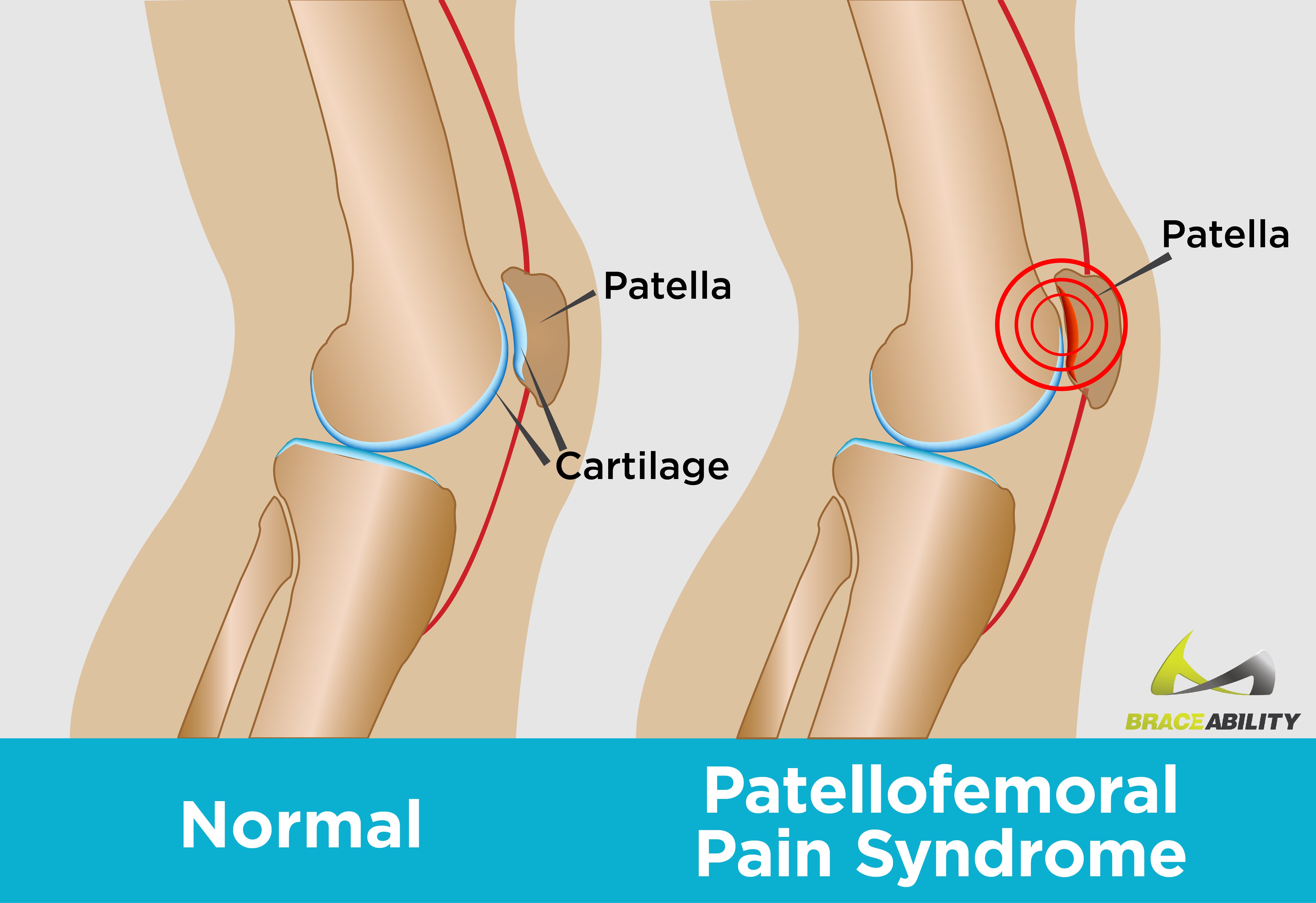
What is Patellofemoral Pain Syndrome?
Patellofemoral pain syndrome (PFPS) refers to pain located in the front of your knee and around your kneecap. It is a very common knee injury, which occurs when your patella (kneecap) comes in contact and rubs with your femur (thigh bone).
Patellofemoral pain syndrome is common among runners and other athletes. You may have heard of it more commonly referred to as runner’s knee or jumper’s knee. However, anyone can experience patellofemoral pain syndrome. Aside from athletes, it is especially common among teenagers, young adults, women, and older adults who have arthritis of the knee.
Patellofemoral pain syndrome affects twice as many women as men. This is likely because women tend to have wider hips, resulting in a greater angle at which the bones in their knee joint meet. The increased angling of a woman's thighbone to her knee puts her kneecap under more stress and results in patellofemoral pain.
Patellofemoral Pain Syndrome Symptoms
Symptoms of patellofemoral pain syndrome may vary among individuals. The onset of pain and other symptoms may be gradual or the result of a single incident.
How Do I Know if I Have Patellofemoral Pain Syndrome?
- Your knees hurt or feel stiff when you climb stairs, squat, sit down, etc.
- You feel a sharp or aching pain around your kneecap
- Your knees feel like they are inflamed or grinding
- Your knees are sore after sitting for a long time
- You hear popping or cracking sounds in your knees
Patellofemoral Pain Syndrome Vs. Chondromalacia Patella
In many cases of patellofemoral pain syndrome, a condition called chondromalacia patella is present. Chondromalacia patella is commonly confused with patellofemoral pain syndrome because many cases of chondromalacia patella result in patellofemoral pain. However, both of these conditions can occur independently of each other.
In comparison to patellofemoral pain syndrome, chondromalacia patella refers to the softening and degeneration of the cartilage located below your kneecap. In other words, chondromalacia patella is an acute knee condition in which the cartilage under your kneecap breaks down. In relation to patellofemoral pain syndrome, chondromalacia can cause bilateral pain (pain around your kneecap) or pain specifically behind your kneecap. Find treatment options for chondromalacia here.
What Causes Patellofemoral Pain Syndrome?
Specifically pinpointing the exact cause of patellofemoral pain syndrome is difficult. However, there is a wide variety of probable causes from biomechanical problems to muscular issues. Most physicians believe patella pain is initially caused by overuse and vigorous physical activities that put repeated stress on your knees, such as jogging, squatting, or climbing stairs.
If you suffer from patellofemoral pain, you should stop doing the activities that make your knee or knees hurt until you are no longer in pain. Many individuals experience less knee pain by simply switching up their exercise routine. One of the best physical activities you can do if you have patellofemoral pain syndrome is swimming because your body floats, and there is no extra pressure placed on your joints or muscles.
Why Do I Have Patellofemoral Pain Syndrome?
- Overuse and repeated stress on your knees
- A sudden change in your exercise routine
- A direct injury, impact, or hit to your knee
- You have poor kneecap alignment
- Problems with your feet, such as flat feet (fallen arches) or high arches
- Your muscles are weak or unbalanced
7 Best Ways to Treat Patellofemoral Pain
You can relieve your patellofemoral pain by avoiding any activities that make your symptoms worse. Fortunately, there are a number of non-surgical ways to alleviate patellofemoral pain syndrome and lead you to rehabilitation.
1. REST AND ICE.
One of the simplest treatment options for patellofemoral pain is rest. You should modify or avoid activities that increase knee pain, such as squatting, climbing stairs, or sitting with your knees bent for long periods of time. In addition, icing your knee after exercise usually helps improve pain. The RICE method (Rest, Ice, Compression, and Elevation) has proven beneficial for many people struggling with patellofemoral pain syndrome. Following this protocol can help reduce swelling, enhance blood flow, and promote healing following exercise.
2. MEDICATIONS.
By taking anti-inflammatory drugs (NSAIDs), including ibuprofen or naproxen, you can relieve many painful symptoms, such as stiffness or swelling.
3. PHYSICAL THERAPY.
A physical therapist may observe the alignment of your feet, analyze your walking and running form, and test the strength of your thigh and hip muscles to find out if there is a weakness or imbalance that might be causing your patellofemoral pain. To safeguard your knees, your physical therapist can show you how to adjust your daily activities and exercise regime.
4. EXERCISES.
Certain exercises can help strengthen your muscles, which support your knees and improve alignment. Most exercises that improve patellofemoral pain focus on strengthening, gently stretching, and foam rolling your quadriceps, hamstrings, and the muscles around your hips. By adding strengthening and stretching to your routine, you may be able to treat or avoid patellofemoral pain syndrome.
Poorly conditioned quadriceps and tight hamstrings are common among many people who suffer from patellofemoral pain syndrome. Weak quadriceps are unable to support your kneecap, leading it to track out of alignment. Whereas, inflexible hamstrings can put added pressure on your knee.
Stretching can prevent tight muscles. If you have tight muscles, that could be why your knees are sore or stiff after running, cycling, etc. Although stretching is very beneficial, sometimes stretching alone is not enough. Using a foam roller to “roll out” the muscles attached to your knees can help with proper alignment of your joints, prevent joint pain (arthralgia), enhance your flexibility, and avoid dysfunction of your knees. Find more information and specific foam roller exercises for the knee here.
5. TAPING.
Patella taping may help reduce pain and give you a greater range of motion. Using tape for the patella is an excellent way to relieve the symptoms of patellofemoral pain syndrome and control the position of the kneecap.
6. SUPPORTIVE BRACES.
Orthopedic knee braces or arch supports can help stabilize the kneecap, alleviate patellofemoral pain, and protect against movements that might cause more damage. This might involve wearing knee wraps, knee braces, or knee sleeves while running. These braces provide comfortable and lightweight support to the knee. Many people also choose to wear these products as a way to strap their knee in place, protect their kneecaps from lateral or medial (side to side) movement, ensure proper healing, or simply to prevent patellofemoral pain syndrome.
7. SURGERY.
If nonsurgical treatments are ineffective and pain persists, contact your doctor for a thorough evaluation. They can confirm the diagnosis and rule out other conditions with comparable symptoms. Your doctor may recommend surgery as a potential treatment option. Fortunately, surgical treatment for patellofemoral pain is rarely needed and only done in severe cases. Most people find relief from the many nonsurgical treatment options listed previously.
Top 4 Patellofemoral Pain Syndrome Prevention Methods
In addition to the patellofemoral pain syndrome treatment tips listed above, there are several other ways you can prevent patellofemoral pain from striking again.
1. WEARING APPROPRIATE SHOES.
One simple solution includes wearing the correct shoes for your body. You should talk to your doctor to make sure your shoes are not doing more harm than good. Make sure your shoes fit well and provide good shock absorption. The best athletic footwear will support the foot and arch. If you have flat feet, consider trying shoe inserts. Shoe inserts can help stabilize and align your foot and ankle, relieving your lower legs and knees of stress.
2. WARM UP AND STRETCH.
Another important prevention method is to warm up and stretch before you exercise. Warming up thoroughly before and after physical activity has proven to reduce and prevent patellofemoral pain. Your warm-up should increase blood flow to your muscles and your loosen joints. By gradually increasing your heart rate and circulation, your body will be better prepared for more strenuous exercise. Stretching your muscles prior to exercise helps prevent injuries and prepares your muscles for physical activity.
3. LOSE WEIGHT.
Being overweight or obese can be really tough on your knees because our knees frequently serve as the shock absorbers for our bodies. Those extra pounds add to the stress on your knees, which can cause patellofemoral pain and lead to more serious complications.
When walking across level ground, the force on your knees is about 1.5 times your bodyweight. For example, a 200-pound individual will put 300 pounds of pressure on their knees with each step as they walk across level ground. Add an incline, and the pressure on their knees is even greater. Furthermore, the force on each knee is 4 to 5 times your body weight every time you squat.
Fortunately, dropping just a few pounds can make a huge difference in your knee pain and may even prevent patellofemoral pain syndrome. Losing weight reduces the amount of pressure on the knee joint, prevents cartilage from wearing down, and relieves stress on your knees.
4. LISTEN TO YOUR BODY.
Finally, it is extremely important to listen to your body. Ignoring chronic knee pain and continuing intense workouts can cause extensive damage in the long run. Make time to rest and recover if you experience knee pain. It is much easier to make a full recovery if patellofemoral pain syndrome is caught and treated. Timely treatment by your doctor or physical therapist may help catch any underlying problems before they worsen and cure your patellofemoral pain. If you are experiencing serious knee pain, please consult with your physician about any concerns or questions you may have.