Going From Prolapse to Powerful: The Complete Guide to Uterine Prolapse
What is a Prolapsed Uterus?
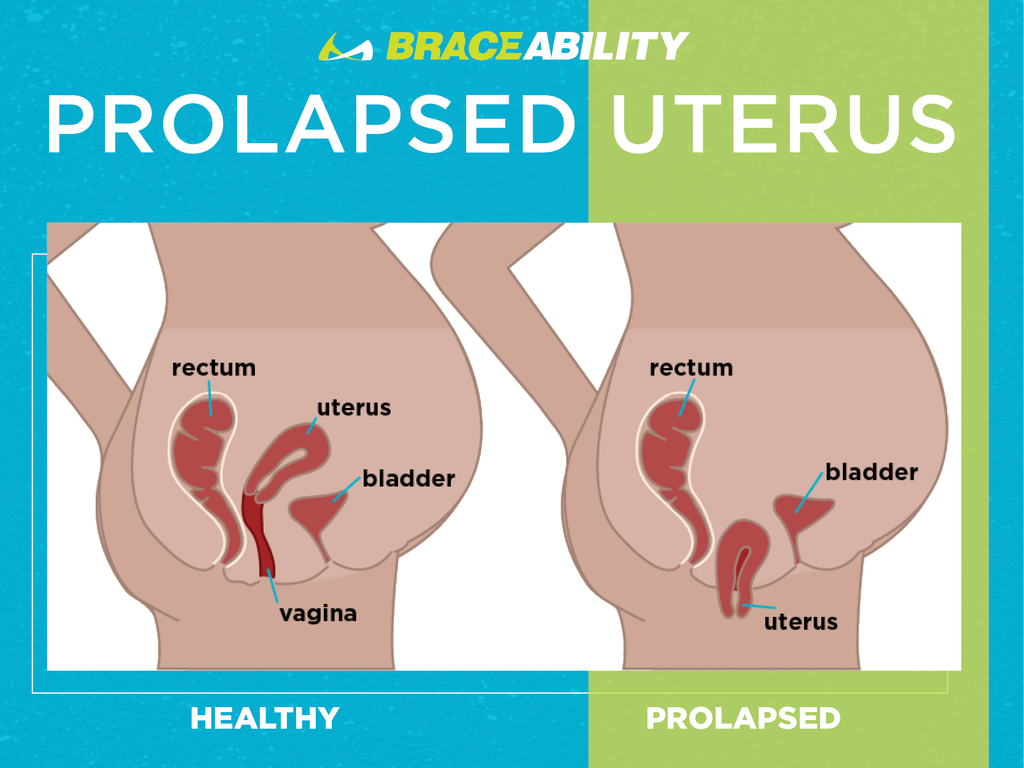
Uterine prolapse is widely known, but how much do you really know about this condition? Prolapse of the uterus occurs for women when the uterus, also known as the womb, descends toward or into the vagina. Essentially, your muscles and ligaments surrounding your uterus, also known as your pelvic floor muscles, become weak and are no longer able to support your uterus. In some cases, the uterus may actually protrude from the vagina. Uterine prolapse is a common condition that can happen to women for a number of reasons.
What Are The Pelvic Floor Muscles?
This group of muscles stretch like a hammock from the pubic bone at the front to the tailbone at the back and side to side from one sitting bone to the other. A woman's pelvic floor muscles support her bladder, bowel and uterus.

Fast Facts on Prolapsed Uterus
- Uterine prolapse is relatively common, especially for women who are over the age of 55.
- The main risk factors include a female who has a high body mass index or has completed menopause, pregnancy and childbirth.
- Kegel exercises are one of the best ways to treat mild forms of uterine prolapse
- Urine leaks, pain in your pelvic area and lower back pain are leading symptoms for a prolapsed uterus.
Did You Know That Uterine Prolapse Can Occur for Animals?
Similar to humans, uterine prolapse can occur for animals as well! Prolapse of the uterus can occur in just about any species, however, for animals, it is most common in dairy and beef cows. The uterus prolapse is most likely to occur immediately after or within several hours of birth delivery when the cervix is open and the uterus lacks tone. Uterine prolapse can also occur in smaller animals such as cats and dogs, although it is very rare.
What Does a Prolapsed Uterus Look Like?
So, how can you tell if your uterus has dropped or is dropping? Uterine prolapse comes in stages or grades, based on the level of severity. The level of severity ultimately depends on how far the uterus drops. It is possible that you have mild uterine prolapse, which can only be seen by your doctor while performing a pelvic exam. There are, however, some severe cases where your uterus may actually protrude out of your vagina. In this case, the uterus will be visible from the outside of the vagina.

Types of Prolapsed Uterus
Uterine prolapse can be classified as either incomplete or complete.
What exactly do these classifications mean?:
- Incomplete uterine prolapse: this occurs when the uterus is partially fallen into the vagina but is not protruding
- Complete uterine prolapse: this occurs when a portion of the uterus protrudes from the vaginal opening
The Stages of a Prolapsed Uterus
Uterine Prolapse is looked at in stages in order to determine the severity and overall how far or low the uterus falls into the vagina. The four stages or grades of Uterine Prolapse are as follows:
-
Stage 1
The uterus is in the upper half of the vagina.
-
Stage 2
The uterus has now descended nearly into the opening of the vagina
-
Stage 3
The uterus has protruded out of the vagina
-
Stage 4
The uterus is completely out of the vagina

Prolapsed Uterus Symptoms
Symptoms will vary based on the severity of the prolapse.
The most typical signs that you may be experiencing a collapsed uterus include:
- Vaginal bleeding or an increase in vaginal discharge
- Pelvic heaviness or pulling
- Difficulties or pain with sexual intercourse
- Urinary leakage
- Bladder infections
- Lower back pain
- Sensations of sitting on a ball or that something is falling out of your vagina
- Constipation or other bowel movement difficulties
- Discomfort when walking
What Causes a Prolapsed Uterus?
Your uterus is held into place within the pelvis by a group of muscles and ligaments, known as your pelvic floor muscles. When these muscles weaken, they are no longer able to hold your uterus in place, causing it to sag. The pelvic floor muscles can weaken for a number of reasons, such as:
- Pregnancy
- Factors relating to childbirth delivery
- Getting older, especially after menopause
- Frequent heavy lifting
- Chronic coughing
- History of pelvic surgery
- Genetic factors
Who is Most Likely to Experience Uterine Prolapse?
The uterus can drop into the vagina due to the reasons listed above, however, it is most likely to occur for women who:
- Those in postpartum who had more than one vaginal delivery, especially for those who have given birth to large babies.
- Are post-menopausal. Estrogen is no longer produced after this time and is a hormone that helps keep your pelvic muscles strong.
- Have family members who have experienced pelvic prolapse.
How is a Prolapsed Uterus Diagnosed?
The diagnosis of a prolapsed uterus will generally occur during a pelvic exam. It is likely that during your pelvic exam, your doctor will ask you to:
- Crouch down, as if you are having a bowel movement. This will help your doctor assess how far your uterus has slipped into the vagina
- To tighten your pelvic muscles, as if you are attempting to stop a stream of urine. This test is done to check the strength of your pelvic floor muscles
Preparing for Your Pelvic Exam Appointment
If you are experiencing symptoms of uterine prolapse, it is likely that you will need to make a visit to your doctor, so that you can receive a pelvic exam. When you are experiencing uterine prolapse, or predict that you may be, it can be a scary and overwhelming time. Before your appointment, make sure you:
- Make a list of all of the questions you have for your doctor
- Discuss all of your treatment options with your doctor and list the pros and cons of each
- Let your doctor know of any pain and or painful experiences you have had in relation to your pelvic or cervical area
- Work on the things you can do to improve your pelvic floor muscles at home beforehand
Complications of a Prolapsed Uterus
While mild uterine prolapse usually doesn’t require treatment, unless you are able to benefit from it, there are some further complications that uterine prolapse could be associated with. Uterine prolapse is often associated with the prolapse of other pelvic organs. You may experience other dangerous conditions such as:
- Posterior Pelvic Prolapse - Also known as rectocele, this is the weakness of connective tissue that separates the rectum from the vagina, which may cause the rectum to bulge into the vagina. If you experience this condition, you will notice difficulty when producing bowel movements.
- Anterior Prolapse - Also known as cystocele, this is the weakness of connective tissue that separates the bladder from the vagina, which may cause the bladder to bulge into the vagina. This is also known as a prolapsed bladder.
If it is needed and you do not treat uterine prolapse, it can ultimately impact your other organs within your pelvic area. An untreated prolapsed uterus can cause life-long problems, as well as interfere with your bowel, bladder, and sex life by causing you pain.
Top 5 At-Home Remedies:
It is unlikely that a uterine collapse will heal itself, luckily, there are some simple steps you can take to reduce your risk of uterine prolapse or simply stop it from worsening, right in the comfort of your own home.
-
Perform Kegel Exercises - The Right Way!
Yes, there is a right and wrong way to perform kegel exercises! Strengthening your pelvic floor muscles is one of the most effective ways to avoid uterine prolapse. Oftentimes, kegel exercises are done incorrectly, which essentially won’t do anything to actually benefit you, or your pelvic floor muscles. Learn how to correctly perform kegel exercises later on in this article!
-
Prevent and Treat Constipation
Constipation and bowel movement problems can greatly worsen a prolapsed uterus. Drink more liquids, eat foods that are high in fiber, get in some exercise regularly or resort to over-the-counter constipation relief in order to avoid these issues.
-
Manage Chronic Coughing
Coughing forces your pelvic floor to move downwards. Repetitive and forceful coughing can stretch and weaken pelvic floor tissues and increase your prolapse severity. See tips below on how to manage your cough while dealing with uterine prolapse.
-
Focus On Your Health
Maintaining a healthy weight and diet can benefit you in so many different ways. By controlling what you eat, you are able to focus on foods that will help you choose foods that are high in nutrients and fibers. Obese women are also more at risk for uterine prolapse.
-
Use Proper Form When Lifting Heavy Objects
Using correct body mechanics whenever lifting heavy objects is going to be key to avoid worsening your uterine prolapse. Heavy lifting is known to be hard on your uterus. Avoid repetitive heavy lifting when possible, especially after pelvic surgery or childbirth.
Treatment Options
On top of the at-home remedies, such as performing kegel exercises, you may also consider some strategies that will require some medical professional help, such as:
- Getting a pessary placed - this will work to hold your uterus in the correct spot
- Surgery to repair your weakened pelvic floor muscles
- Hysterectomy - the removal of your uterus
- Wear a support belt - this is a brace that is usually applied like underwear and will work to hold your uterus in the correct spot, as well as treat other similar conditions such as vulvar varicose veins
Talk with your doctor, consider all of your treatment options and the risks and benefits associated with each option before choosing what will work best for you.
What Will Surgery Look Like For a Prolapsed Uterus?
If natural treatments to heal uterine prolapse are not working, you may need to have your uterus removed. The procedure of removing your uterus is known as a hysterectomy. This can be done in two different ways:
- Vaginal Hysterectomy - This procedure includes an incision made in the vagina, the surgeon will then detach the uterus from the ovaries, fallopian tubes, upper vagina and connective tissues, therefore completely removing the uterus.
- Abdominal Hysterectomy - This is the same procedure as the vaginal hysterectomy, but the incision is made in the abdomen and the uterus is removed through this method.
Can I Surgically Repair My Prolapse Without a Hysterectomy?
Yes! There is a procedure you can have performed that works to repair your uterine prolapse without the need to completely remove it. This procedure involves putting the uterus back into its normal position. This is called uterine suspension and may be done by reattaching your pelvic ligaments to the lower part of the uterus in order to hold it into place. This surgery can either be done through the vagina or through the abdomen based on whichever technique is used.
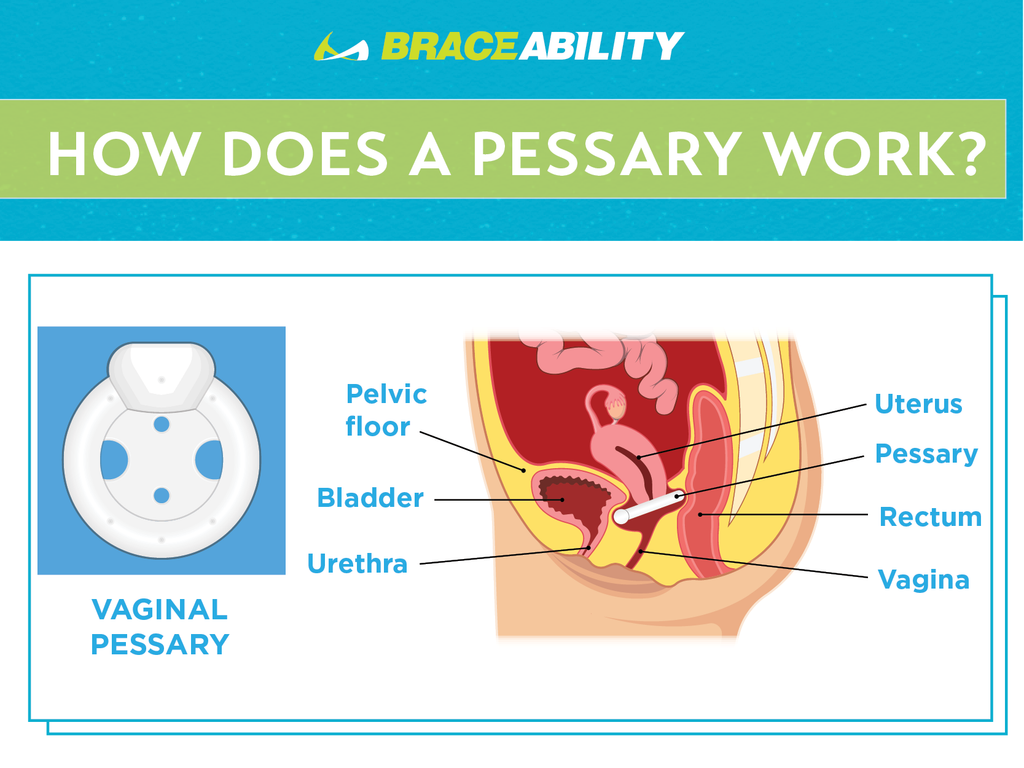
What is a Pessary?
A pessary is a soft rubber or plastic removable ring that is inserted into your vagina in order to support the bulging tissues that were affected by the prolapsed uterus. Essentially, the device will hold your uterus in place. There is a range of options when it comes to vaginal pessaries. When it comes to deciding which pessary is right for you, It is likely that your doctor will be able to make the best recommendation for you based on the issues you are having with your condition
Your doctor will fit you with several different pessaries, ranging in size until he or she finds one that fits you best. The pessary must be in the right position and be the right size for you in order to be able to do its job! After your first fitting, you will need to return to your doctor in order to have the pessary rechecked. You will likely have a recheck appointment every few months.
How Do I Take Care of My Pessary?
Taking care of your pessary and listening to your doctor's instructions is SO important. All pessaries will need to be cleaned, but it will depend on the type of pessary you have as to how often it should be cleaned. For most pessaries, you can take them out yourself and you can wear them many days before they need to be cleaned.
To clean your pessary, you can use simple soap and water, dry the pessary completely and reinsert it the following morning. Keep in mind that this will only be necessary if your doctor has given you the okay to take your pessary out yourself.
Why Do Kegel Exercises Matter?
Your pelvic floor muscles can be weakened and strained by many factors. Pregnancy, childbirth, aging, surgery and many more cause excessive straining to your pelvic floor. These muscles support your urethra, bladder, uterus and rectum. Performing kegel exercises will provide an easy fix for those weakened pelvic floor muscles!
Having strong pelvic floor muscles can:
- Reduce urine leakage due to urinary incontinence
- Increase muscle strength for childbirth
- Ease your recovery after pregnancy
Keep in mind that you will need to be patient, as the changes that kegel exercises make can take up to 3-6 weeks.
How Do I Perform Kegel Exercises Correctly?
Kegel exercises can be extremely helpful in strengthening your pelvic floor, however, if you aren’t doing the exercises correctly, you won’t reach those desired results. Kegels are easy to do, risk-free and painless. The main issue that arises when performing kegel exercises is that you are not identifying and working the correct muscles.
To identify the correct, pelvic floor muscles:
- Stop your urination midstream
- The muscles you feel being used when this occurs are your pelvic floor muscles, which is what you will need to set your focus on in order to strengthen them during your kegel exercises
How to Do Kegel Exercises
- Make sure your bladder is empty, then sit or lie down
- Tighten your pelvic floor muscles, hold this tightly and count 3 to 5 seconds
- Relax your muscles and count 3 to 5 seconds
- Repeat this 10 times through, 3 times a day (morning, afternoon and night)
For the best results, you will need to maintain your focus. Focus on tightening only your pelvic floor muscles. Avoid flexing the muscles in your abdomen, thighs, or buttocks. Avoid holding your breath. Instead, breathe freely during the exercises.
Can I Use Physical Therapy to Help With My Prolapse?
Absolutely! This is something that is actually highly recommended by a lot of doctors in order to ease any pain you may be feeling, as well as strengthening your pelvic floor muscles. Pelvic physical therapy is known to delay or prevent surgery. If the timing is right, you could avoid having to have surgery performed altogether.
Treatment through physical therapy is a multi-pronged approach. The most common pelvic physical therapy steps usually include:
-
Taking the pressure off of your pelvic floor
Your physical therapist will assess your lifestyle and prescribe a restriction on carrying heavy loads. The goal with this step is to ultimately reduce downward pressure on the pelvic floor muscles.
-
Assuring sure you have the correct pelvic alignment
Before you can build up strength on your pelvic floor, your physical therapist is going to want to make sure that you have the correct pelvic alignment. The reason being that your muscles can not be properly strengthened if the alignment is off.
-
Learning to breathe properly
It is likely that your physical therapist is going to stress the importance of breathing mechanics early on in your treatment. When tightening or relaxing muscles, it is important that you are inhaling and exhaling in the correct corresponding ways to avoid additional downward pressure on your pelvis.
-
Strengthening your supporting core muscles
The obvious goal when treating pelvic organ prolapse is to strengthen your pelvic floor muscles. This is done by a combination and coordination of the first three steps mentioned above. Once these have been addressed, your physical therapist will begin to work on strengthening other core muscles such as your glutes, hip stabilizers and other abdominal muscles. This will ultimately help to improve your posture, assuring that everything you’ve worked for up to this point continues to stay aligned and strong.
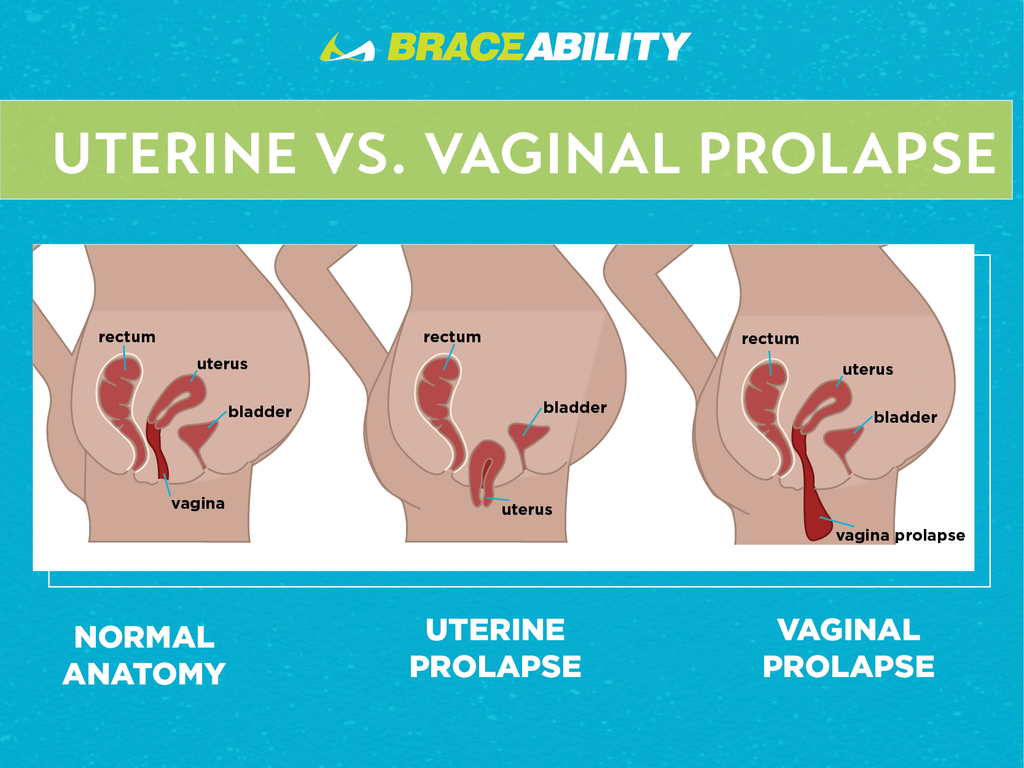
Prolapsed Uterus vs Vaginal Prolapse: What’s the Difference?
These two conditions can often be confused, yet are actually quite different. We now know that with uterine prolapse, your uterus has sunk down out of its normal place. Similarly, vaginal prolapse occurs when the vagina slips out of position. Your vagina is one of several organs that rests in the pelvic area of your body. These organs are held in place by muscles and other tissue. The same way your pelvic floor muscles weaken causing uterine prolapse can also cause vaginal prolapse.
Is a Prolapsed Uterus Possible While You’re Pregnant?
Uterine prolapse complicating pregnancy is very rare, in fact so rare that the chances of it happening are 1 in 10,000-15,000 pregnancies. Though it’s unlikely that this will occur, it is important you seek medical help and attention as soon as you begin experiencing symptoms of a collapsed uterus. Very careful assessment is required in order to prevent complications during delivery. If this ends up being the case for you, it is likely that your best and safest option will be to have your delivery through a cesarean section. Make sure you discuss your options with your physician to find what is going to work best for you and your baby before making any decisions!
Tips for Dealing With a Prolapsed Uterus
The best thing you can do for your health while dealing with uterine prolapse is to make any lifestyle changes necessary in order to improve and work on strengthening your pelvic floor. Any added pressure to your pelvic floor muscles can drastically worsen the stage of your prolapse.
The top strategies include avoiding the lifting of heavy objects. The exertion that is applied when lifting heavy objects, especially with the wrong form can be hard on your pelvic floor. Another action that can add pressure to this area is repetitive coughing. Avoid smoking and any other factors that may worsen your cough.
Lastly, the best thing you can do is watch what you eat to ensure you are constantly working to improve your overall health and weight. Eat healthy foods and perform exercises, including your kegels, daily. Doing these things can affect the improvement of your pelvic floor greatly, which in turn will have a positive impact on the improvement of your uterine prolapse.